Impact Of Blood Pressure Conditions On Coronary Perfusion And Hemodynamics After Aortic Valve Replacement
Brennan Vogl1, Scott Lilly2, Vinod Thourani3, Mohamad Alkhouli4, Brian Lindman5, Hoda Hatoum1.
1Biomedical Engineering Department, Michigan Technological University, Houghton, MI, USA, 2Department of Cardiovascular Medicine, The Ohio State University, Columbus, OH, USA, 3Department of Cardiovascular Surgery, Piedmont Heart Institute, Atlanta, GA, USA, 4Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, USA, 5Department of Cardiovascular Medicine, Vanderbilt University School of Medicine, Nashville, TN, USA.
Objective: It has been recently reported that lower systolic and diastolic blood pressures (SBP, DBP) for patients with aortic valve replacement (AVR)—in the range that is currently recommended as the optimal target in blood pressure (BP) guidelines (SBP <e; 120-130mmHg and DBP <e; 80mmHg)—are independently associated with an increased cardiovascular mortality. The aim of this work is to evaluate the impact of various BP conditions on the coronary perfusion and hemodynamic performance after AVR. Methods: The hemodynamic assessment of a 26mm SAPIEN 3 transcatheter aortic valve (TAV), 29mm Evolut R TAV, and 25mm Magna Ease surgical aortic valve (SAV) was performed in a pulsed left heart simulator with varying SBP, DBP at 60bpm. The total coronary flow (CF) was initialized for the experiments at 120/60mmHg and left to vary based on the different BPs. The average CF and effective orifice areas (EOA) for each valve were calculated. Sinus washout calculations were performed on the SAPIEN 3 to see how blood pressure can affect sinus hemodynamics. Results: As SBP and DBP increased, there was a trend of increasing CF from 100/60 to 180/60mmHg and from 120/40 to 120/90mmHg with all valves. EOA was found to decrease with an increasing SBP and DBP. Sinus washout was quickest with the highest SBP. The results can be seen in Figure 1. Conclusion: Increasing SBP and DBP yielded improvements to coronary perfusion but also decreased EOA, independently from valve type. In addition, sinus washout also improved with an increase in SBP. This emphasizes the need for additional studies to identify the ideal blood pressure target post-AVR and to further understand the basis of worsening outcomes with lower blood pressure conditions in these patients. 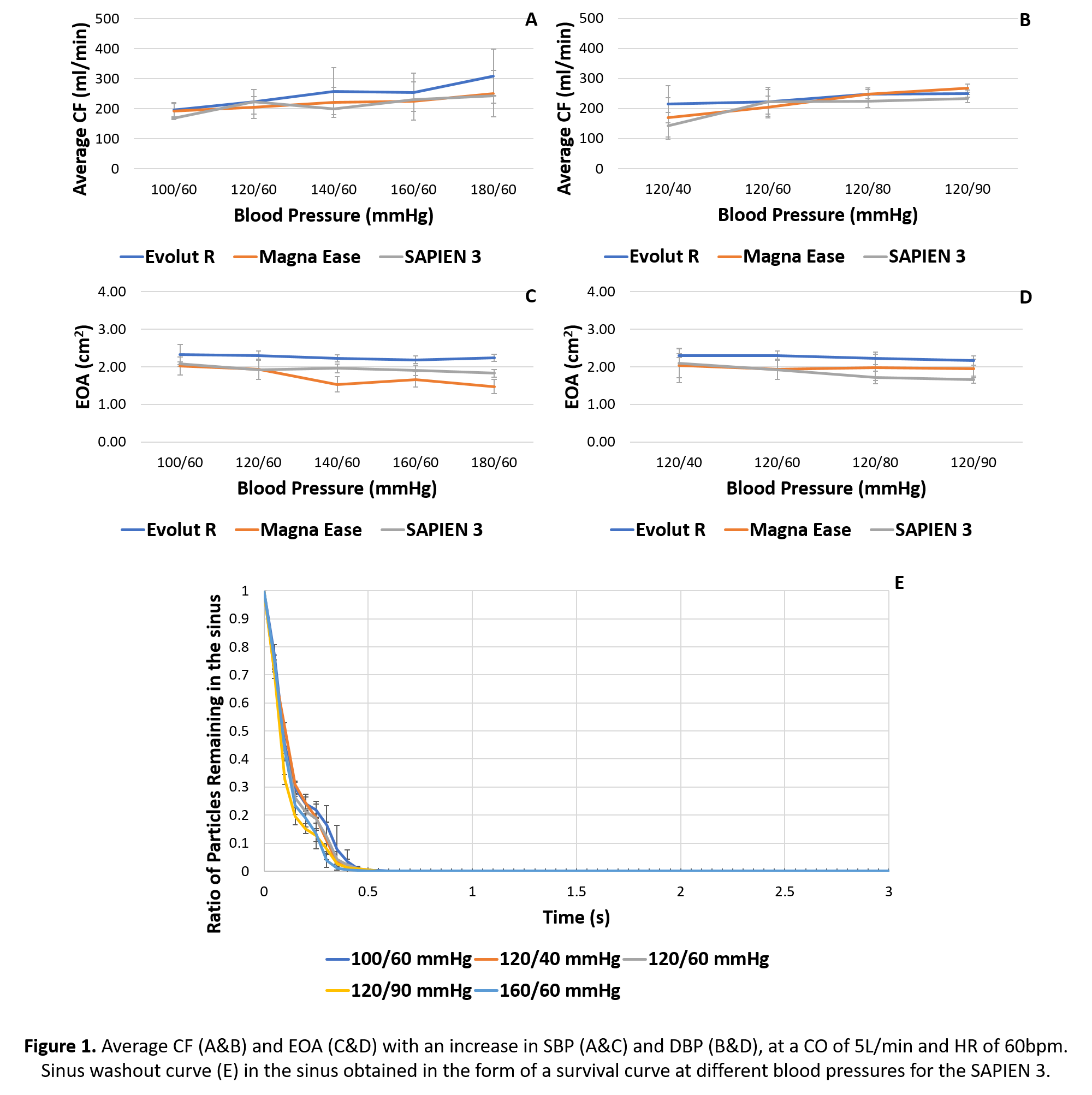
Back to 2022 Abstracts
